When I went to the doctor years ago for help with my concussion symptoms and mental health challenges, he offered me two options – addictive sleeping pills or antidepressants.
That was it.
I was left in the dark.
I had no other options and nowhere to turn, so I had to take the medication.
Years later, I now know there are many other options and solutions.
N-acetyl-cysteine (NAC), a cheap amino acid and antioxidant, is an effective way to deal with the root cause of mental illness and sub-optimal cognition.
What's N-Acetylcysteine? How Can It Help The Brain?
N-acetyl-cysteine (NAC) is a modified form of the amino acid cysteine and helps your body produce glutathione.
Glutathione is a powerful antioxidant that supports liver detoxification and reduces free radicals in the body.
Over the past 30 years, high doses of NAC have been used in emergency rooms to combat acetaminophen (Tylenol) toxicity (1, 2).
But there is also an overwhelming amount of evidence showing that NAC can help treat a number of neurological and psychiatric disorders, and it helped me years ago when I was trying to recover from mental illness and post-concussion syndrome.
A systematic review of all of the evidence suggests that NAC is effective at treating the following conditions (4, 6, 18, 19):
• Major depressive disorder
• Bipolar disorder
• Drug addiction
• Obsessive-compulsive disorder
• Autism
• Schizophrenia
• Alzheimer's disease
• Certain forms of epilepsy (progressive myoclonic)
NAC also reduces the severity of mild traumatic brain injury in soldiers, and animal studies show that it can improve cognition after moderate traumatic brain injury (5).
Disorders such as anxiety and attention deficit hyperactivity disorder have preliminary evidence but require larger studies (4, 6).
Overall, it’s clear to me that NAC should be a first-line treatment for mental illness.
My recommendation: I used to take 1200 mg of NAC every day to manage my long-term mental health. It was very helpful at one point in time. I no longer need to take it anymore because I’m completely recovered and well. It’s just not necessary for me anymore because I’m healthy. However, when I was taking it, I eventually started experienced some side effects due to heavy metal redistribution. Studies show that people benefit from taking anywhere between 500 mg to 3000 mg daily or every other day. But I find that many people actually do better when they take a lower dose because high doses of NAC can sometimes redistribute heavy metals into the brain. You’ll obviously want to avoid this. I now recommend people take just 250 mg of NAC, which can be found in the Optimal Antiox supplement. Optimal Antiox also contains a number of other antioxidants and nutrients that can support your brain and mental health. Optimal Antiox also includes leucine, which is an amino acid. Taking leucine with NAC prevents mercury from being reabsorbed into the central nervous system.
How Is It So Effective At Treating All These Mental Health Conditions?
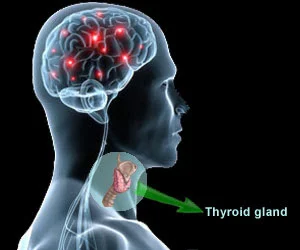
First of all, it's important to note that NAC seems to target biological pathways that are common across all mental disorders.
Here are some possible explanations for its effectiveness:
NAC has anti-inflammatory properties, and inflammation has been linked to depression and other mental health disorders (12, 13).
NAC has also been shown to successfully cross the blood-brain-barrier and raise glutathione levels in the brain. Low levels of glutathione in the brain have been linked to a number of psychiatric disorders (8-11, 17-19, 24).
High levels of oxidative stress have been identified in the brains of patients with a variety of psychiatric illnesses. Increasing brain glutathione by supplementing with NAC can help reduce this oxidative stress and protect neurons from oxidative damage (20-23, 25).
Lastly, NAC may be having beneficial effects on patients by reducing glutamate, a major excitatory neurotransmitter in the brain that can lead to overstimulation (14-16, 26).
Therefore, if you take NAC, you're giving your body an efficient way to soak up excess glutamate. You’re also reducing oxidative stress and inflammation by giving it glutathione. As a result, this helps alleviate a number of different mental health problems.
Below, I’ll lay out some of the research exploring NAC as a possible treatment for six mental health problems. Feel free to skip to your condition to learn about it.
Depression and Bipolar Disorder
Here is some of the research looking into NAC as a possible treatment for depression and bipolar disorder:
A randomized controlled trial examined 149 individuals with moderate depression. They received two grams of NAC or placebo. Before treatment, the estimated mean depression score was 19.7. At the end of the 8-week study, the score had decreased to 11.1. Individuals who received NAC witnessed improvements in functioning and quality of life (27).
Another randomized controlled trial looked at 75 patients with bipolar disorder. Two grams of NAC or placebo was given for 6 months. At the end of this period, the group who received NAC saw a reduction in their depression and significant improvements in their global, social and occupational functioning. The improvements were rated as “medium to high” and it was concluded that "NAC is a safe and effective augmentation strategy for depressive symptoms” (28).
Several other studies have examined the effects of NAC on bipolar disorder (including mania) and found that two grams of NAC daily significantly improves and even causes a full remission of both depressive and manic symptoms (29-31).
It’s important to note that some of these studies lasted 6 months, which is a very long time for randomized control trials. And all of the studies had beneficial effects and zero severe side effects. That’s quite impressive.
All of the above research makes sense in light of a meta-analysis that found that patients with bipolar disorder have significantly higher levels of oxidative stress and glutamate in their brain.
A number of mood-stabilizing medications aim to decrease glutamate, yet they come with numerous side effects (14-16, 26, 27, 32, 33).
And as I've discussed before, certain antidepressants can deplete glutathione, which further increases oxidative stress.
Addiction
Substance abuse and addiction are very costly. Yet there are hardly any efficient treatments that prevent relapse.
But a lot of research is emerging demonstrating a link between oxidative stress and drug addiction, and how NAC can help manage it (66-68).
In a small study, 13 people abstaining from cocaine were given 2,400 mg of NAC or placebo over two days. The participants who received NAC witnessed a significant reduction in their withdrawal symptoms and cravings for cocaine (34). Follow-up studies also showed that NAC reduced desire and interest in cocaine (35, 36).
Smokers voluntarily reduce their cigarette use by around 25% after two weeks of supplementing with 2,400 mg of NAC (37, 65).
And it’s not just addiction to drugs. NAC also shows promise for the treatment of gambling addiction. A randomized control trial with 27 pathological gamblers showed that gamblers who supplemented with NAC scored 60% lower on the “Obsessive Compulsive Scale for Pathological Gambling." (38).
Here are 8 other nutrients that can help with addiction.
Obsessive-Compulsive Disorder (OCD)
Not surprisingly, there are brain similarities among people who suffer from addiction and obsessive–compulsive disorder (OCD).
Just like addiction, higher levels of oxidative stress and glutamate are found in people with OCD (39-44).
The standard treatment for OCD is a combination of antidepressants and psychotherapy.
But around 20% of patients don’t get better with this combination, and many suffer from a variety of drug side effects (45).
Since NAC is inexpensive and widely available, it’s clear that it has significant advantages for patients.
I also encourage you to check out this article for 21 other ways to treat OCD.
Autism
Autism is a touchy subject. So let me start out by saying that NAC will not cure autism. Autism has many different causes and contributing factors.
However, NAC will likely improve some autistic symptoms.
Multiple studies suggest that NAC is a well-tolerated treatment for autistic individuals and can reduce their irritability (46-48).
Like the disorders above, research has found that autistic individuals have higher levels of oxidative stress and lower levels of the antioxidant glutathione in their brains, making it likely that NAC will help them (49-55).
There is also lots of evidence suggesting that too much glutamate in the brain contributes to autistic symptoms. As discussed earlier, glutamate in a major excitatory neurotransmitter in the brain. It is also the precursor to GABA, a calming neurotransmitter that reduces anxiety.
There is an enzyme that converts glutamate to GABA, and researchers have found that this enzyme is lower in individuals on the autism spectrum. This leads to more glutamate and less GABA, and therefore much more excitation. Not surprisingly then, glutamate antagonists (e.g. NAC) have been shown to reduce symptoms of autism, bringing them more into balance (56-60).
Since oxidation and glutamate are abnormally elevated in persons with autism, NAC can kill two birds with one stone by providing an antioxidant effect and reducing glutamate levels in the brain of autistic individuals.
Schizophrenia
The last mental disorder I’m going to explore is schizophrenia. There is a good amount of research suggesting that NAC can help with this condition as well.
Researchers gave 2 grams of NAC to schizophrenic patients during a six-month randomized control trial. The participants who received NAC experienced improvements in their symptoms, and many of them did not experience improvements from other treatments. They demonstrated improvements in insight, self-care, social interaction, motivation, and stabilization of mood. Follow-up studies found similar results (62, 63, 70).
I found one study that explored NAC’s ability to change schizophrenic patient’s electroencephalogram (EEG) synchronicity – a measure of electrical activity within the brain that I discussed in my post about neurofeedback (69).
I also found a case report of a young woman with treatment-resistant schizophrenia who showed significant improvements in symptoms by taking just 600 mg of NAC every day (64).
This makes sense considering there is an expanding body of evidence suggesting oxidative stress occurs in individuals with schizophrenia. Some research shows that the more oxidative stress a schizophrenic patient experiences, the worse their symptoms get. And several studies indicate that NAC may benefit schizophrenics by increasing glutathione and reducing glutamate (61, 71-74).
Conclusion
Overall, oxidation and glutamate are often abnormally elevated in people with a wide range of neurological and psychiatric disorders.
NAC may correct these underlying problems by generating the antioxidant glutathione and reducing the excitatory neurotransmitter glutamate.
If you suffer from depression, bipolar disorder, OCD, drug addiction or autism, you could start taking it and see if it helps you. If it helps, keep taking. If not, then try something else.
Many of the studies also suggest that NAC enhances the effectiveness of psychiatric medications. So if you're already on medication, NAC and your medication will likely work better together.
My recommendation: I used to take 1200 mg of NAC every day to manage my long-term mental health. It was very helpful at one point in time. I no longer need to take it anymore because I’m completely recovered and well. It’s just not necessary for me anymore because I’m healthy. However, when I was taking it, I eventually started experienced some side effects due to heavy metal redistribution. Studies show that people benefit from taking anywhere between 500 mg to 3000 mg daily or every other day. But I find that many people actually do better when they take a lower dose because high doses of NAC can sometimes redistribute heavy metals into the brain. You’ll obviously want to avoid this. I now recommend people take just 250 mg of NAC, which can be found in the Optimal Antiox supplement. Optimal Antiox also contains a number of other antioxidants and nutrients that can support your brain and mental health. Optimal Antiox also includes leucine, which is an amino acid. Taking leucine with NAC prevents mercury from being reabsorbed into the central nervous system.
References:
1. http://www.ncbi.nlm.nih.gov/pubmed/677146/
2. Atkuri, K.R., et al. “N-Acetylcysteine — a safe antidote for cysteine/glutathione deficiency”. Current Opinion in Pharmacology Vol. 7, No. 4 (2007): 355–359.
3. http://www.ncbi.nlm.nih.gov/pubmed/16439183
4. http://www.ncbi.nlm.nih.gov/pubmed/25957927
5. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3553161/
6. http://www.ncbi.nlm.nih.gov/pubmed/11673605/
7. http://www.ncbi.nlm.nih.gov/pubmed/12512991
8. http://www.ncbi.nlm.nih.gov/pubmed/2029805/
9. http://www.ncbi.nlm.nih.gov/pubmed/18004285/
10. http://www.ncbi.nlm.nih.gov/pubmed/11691805
11. http://www.ncbi.nlm.nih.gov/pubmed/12603840
12. http://www.ncbi.nlm.nih.gov/pubmed/20021321
13. http://www.ncbi.nlm.nih.gov/pubmed/19122532
14. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3044191/
15. http://www.ncbi.nlm.nih.gov/pubmed/17401648/
16. http://www.ncbi.nlm.nih.gov/pubmed/12584726/
17. http://www.ncbi.nlm.nih.gov/pubmed/12512991
18. http://www.ncbi.nlm.nih.gov/pubmed/24752591
19. http://www.ncbi.nlm.nih.gov/pubmed/25004186
20. Andreazza, A.C., et al. “Oxidative stress markers in bipolar disorder: a meta-analysis”. Journal of Affective Disorders Vol. 111, No. 2–3 (2008): 135–144.
21. Kim, H.K., et al. “Oxidation and nitration in dopaminergic areas of the prefrontal cortex from patients with bipolar disorder and schizophrenia”. Journal of Psychiatry & Neuroscience Vol. 39, No. 1 (2014): 130155.
22. Wang, J.F., et al. “Increased oxidative stress in the anterior cingulate cortex of subjects with bipolar disorder and schizophrenia”. Bipolar Disorders Vol. 11, No. 5 (2009): 523–529.
23. Gawryluk, J.W., et al. “Decreased levels of glutathione, the major brain antioxidant, in post-mortem prefrontal cortex from patients with psychiatric disorders”. The International Journal of Neuropsychopharmacology Vol. 14, No. 1 (2011): 123–130.
24. Holmay, M.J., et al. “N-Acetylcysteine boosts brain and blood glutathione in Gaucher and Parkinson diseases”. Clinical Neuropharmacology Vol. 36, No. 4 (2013): 103–106.
25. Gawryluk, J.W., et al. “Decreased levels of glutathione, the major brain antioxidant, in post-mortem prefrontal cortex from patients with psychiatric disorders”. The International Journal of Neuropsychopharmacology Vol. 14, No. 1 (2011): 123–130
26. Gigante, A.D., et al. “Brain glutamate levels measured by magnetic resonance spectroscopy in patients with bipolar disorder: a meta-analysis”. Bipolar Disorders Vol. 14, No. 5 (2012): 478–487.
27. Berk, M., et al. “The efficacy of N-acetylcysteine as an adjunctive treatment in bipolar depression: an open label trial”. Journal of Affective Disorders Vol. 135, No. 1–3 (2011): 389–394.
28. http://www.ncbi.nlm.nih.gov/pubmed/18534556
29. Magalhães, P.V., et al. “N-Acetylcysteine for major depressive episodes in bipolar disorder”. Revista Brasileira de Psiquiatria Vol. 33, No. 4 (2011): 374–378.
30. Magalhães P.V., et al. “N-Acetyl cysteine add-on treatment for bipolar II disorder: a subgroup analysis of a randomized placebo-controlled trial. Journal of Affective Disorders Vol. 129, No. 1–3 (2011): 317–320.
31. Magalhães, P.V., et al. “A preliminary investigation on the efficacy of N-acetyl cysteine for mania or hypomania”. The Australian and New Zealand Journal of Psychiatry Vol. 47, No. 6 (2013): 564–568.
32. http://www.ncbi.nlm.nih.gov/pubmed/18539338/
33. http://www.ncbi.nlm.nih.gov/pubmed/19568477/
34. http://www.ncbi.nlm.nih.gov/pubmed/16449100/
35. http://www.ncbi.nlm.nih.gov/pubmed/17606664/
36. http://www.ncbi.nlm.nih.gov/pubmed/17113207/
37. http://www.ncbi.nlm.nih.gov/pubmed/19103434
38. http://www.ncbi.nlm.nih.gov/pubmed/17445781
39. http://www.ncbi.nlm.nih.gov/pubmed/12207144
40. http://www.ncbi.nlm.nih.gov/pubmed/19272303
41. http://www.ncbi.nlm.nih.gov/pubmed/16682105
42. http://www.ncbi.nlm.nih.gov/pubmed/18957313
43. http://www.ncbi.nlm.nih.gov/pubmed/18006203
44. http://link.springer.com/article/10.1007/s00213-005-0246-6
45. http://www.ncbi.nlm.nih.gov/pubmed/19468281/
46. http://www.ncbi.nlm.nih.gov/pubmed/23826003
47. http://www.ncbi.nlm.nih.gov/pubmed/22342106
48. http://www.ncbi.nlm.nih.gov/pubmed/23886027
49. http://www.ncbi.nlm.nih.gov/pubmed/21519954
50. http://www.ncbi.nlm.nih.gov/pubmed/22225920
51. http://www.ncbi.nlm.nih.gov/pubmed/22127832
52. http://www.ncbi.nlm.nih.gov/pubmed/16081262
53. http://www.ncbi.nlm.nih.gov/pubmed/22528835
54. http://www.ncbi.nlm.nih.gov/pubmed/21484198
55. http://www.ncbi.nlm.nih.gov/pubmed/22051046
56. http://www.ncbi.nlm.nih.gov/pubmed/21967199
57. http://www.ncbi.nlm.nih.gov/pubmed/22653211
58. http://www.ncbi.nlm.nih.gov/pubmed/17502791
59. http://www.ncbi.nlm.nih.gov/pubmed/22342106
60. http://www.ncbi.nlm.nih.gov/pubmed/22579303
61. http://www.ncbi.nlm.nih.gov/pubmed/18538422/
62. http://www.ncbi.nlm.nih.gov/pubmed/18436195/
63. http://www.ncbi.nlm.nih.gov/pubmed/20868637/
64. http://www.ncbi.nlm.nih.gov/pubmed/19735056/
65. http://www.ncbi.nlm.nih.gov/pubmed/19103434/
66. http://www.ncbi.nlm.nih.gov/pubmed/18440072
67. http://www.ncbi.nlm.nih.gov/pubmed/18996163
68. http://www.ncbi.nlm.nih.gov/pubmed/18225476
69. Carmeli, C., et al. “Glutathione precursor N-acetyl-cysteine modulates EEG synchronization in schizophrenia patients: a double-blind, randomized, placebo-controlled trial”. PLoS One Vol. 7, No. 2 (2012): e29341.
70. https://www.researchgate.net/publication/258347895_N-Acetylcysteine_as_an_Adjunct_to_Risperidone_for_Treatment_of_Negative_Symptoms_in_Patients_With_Chronic_Schizophrenia_A_Randomized_Double-Blind_Placebo-Controlled_Study
71. http://www.ncbi.nlm.nih.gov/pubmed/19689277
72. http://www.ncbi.nlm.nih.gov/pubmed/19576938
73. http://www.ncbi.nlm.nih.gov/pubmed/19788631
74. http://www.ncbi.nlm.nih.gov/pubmed/18205981